Are you worried about how your baby is growing and developing? Maybe you have noticed that your little boy does not look at you when you call his name. Maybe your little girl is not talking or playing with other children. Perhaps your doctor has said that your child’s development is not on track, and you are worried. Maybe your child was developing at a normal rate and then stopped or went backwards.
Could it be autism? Maybe your child has been diagnosed on the autism spectrum. What does autism mean?
Autism is a pattern of differences in a child’s development that affects socialization, communication, play and behavior. Autism is part of a group of pervasive developmental disorders known as Autism Spectrum Disorders (ASD) that significantly impact how a person relates and interacts with others.
As the name implies, ASD is a spectrum disorder that affects individuals differently, and with varying degrees of severity. Autism is neurobiological meaning that the features of autism result from physical differences in a person’s brain and how the person processes information. While autism is a condition that usually lasts throughout a person’s lifetime, people with ASD can and should improve, particularly when their needs are identified and addressed.
This section offers information about child development and the signs of autism in young children. These facts may help you understand what autism is. You may see the ways your child shows the pattern of differences that is called autism. This can help you talk with your doctor if your child has the features of autism but doesn’t have a diagnosis. If your child has a diagnosis, you may better understand how autism affects your child.
Understanding autism can help you accept your child’s condition and find the services or therapies your child may need. This section also helps parents understand the “systems” that offer services for young children so you can navigate these systems as smoothly and quickly as possible. You may have many questions and we hope this section will provide answers, resources, and tools to help.
Child Developmental Differences in Autism
The developmental differences seen in autism can be described as children not doing things we expect them to do, and children doing unexpected things. For example, we expect children to play with toys. We do not expect children to line their toys up in a row instead of playing with them.
To understand these kinds of differences, it helps to understand key stages of a young child’s typical growth and development. Then you can identify any expected things your child is not doing. You may also notice some unexpected things that your child does or says.
You may see signs in different areas or domains: social, communication, behavior, sensory, physical and cognitive/learning. These differences may be closely related to a diagnosis of autism. If your child has a diagnosis, he or she will probably need help to develop in these areas. That is why it is important to identify these differences in your child and share the information with others who can help.
Look at the Picture Dictionary of Child Development. It focuses attention on how babies learn to relate to others, communicate and play. After you read it, you can use the Picture Dictionary Checklist to make notes about any differences that you may see in your child. The checklist has room to write down your examples, questions and concerns.
Red Flags for Developmental Delays
When children do not develop in ways that are expected, especially in several different domains (areas), this can signal the possible presence of a developmental disability like autism. Red Flags for Child Development from birth to age 3 is another helpful tool that describes red flags or warning signs of developmental differences in young children. Please note, this particular list only lists red flags in the areas or domains possibly related to autism, not every possible domain.
You can use Red Flags for Child Development from birth to age 3 to identify areas of concern about your child. If there are several concerns, discuss them with a medical professional. Even without a diagnosis, these types of delays may make a child younger than three years old eligible to receive free Early Start Services through the Regional Center. Click here for more information.
Diagnostic Criteria for Autism
Now that you are familiar with key stages of child development and recognize some of the differences in your own child’s development, the diagnostic features of autism will make sense to you. If your child already has a diagnosis, you will want to know which criteria your child meets. These can become areas of focus to help your child develop skills, now and in the future. Understanding the features can also be helpful if you will be seeking a diagnosis or consulting with your child’s healthcare provider.
There are twelve possible features of autism, representing a “pattern of differences” in the areas of socialization, communication and behavior. To receive the diagnosis, at least SIX criteria must be met out of twelve.
Diagnostic and Statistical Manual-IV, Text Revision (DSM-IV-TR)
The American Psychiatric Association’s Diagnostic and Statistical Manual-IV, Text Revision (DSM-IV-TR) provides criteria to help diagnose Autism. Other criteria are used to diagnose Asperger Syndrome and Pervasive Developmental Disorder-NOS (PDD, or PDD.NOS). Diagnosticians follow guidelines to “rule in” or “rule out” other possible reasons for the child’s differences before giving a diagnosis of autism.
Diagnostic Criteria for 299.00 Autistic Disorder
A. Six or more items from (1), (2), and (3), with at least two from (1), and one each from (2) and (3):
1. Qualitative impairment in social interaction, as manifested by at least two of the following: A) Marked impairment in the use of multiple nonverbal behaviors such as eye-to-eye gaze, facial expression, body postures, and gestures to regulate social interaction B) Failure to develop peer relationships appropriate to developmental level C) A lack of spontaneous seeking to share enjoyment, interests, or achievements with other people (e.g., by a lack of showing, bringing, or pointing out objects of interest) D) Lack of social or emotional reciprocity
2. Qualitative impairments in communication as manifested by at least one of the following: A) Delay in, or total lack of, the development of spoken language (not accompanied by an attempt to compensate through alternative modes of communication such as gesture or mime) B) In individuals with adequate speech, marked impairment in the ability to initiate or sustain a conversation with others C) Stereotyped and repetitive use of language or idiosyncratic language D) Lack of varied, spontaneous make-believe play or social imitative play appropriate to developmental level
3. Restricted repetitive and stereotyped patterns of behavior, interests, and activities, as manifested by at least one of the following: A) encompassing preoccupation with one or more stereotyped and restricted patterns of interest that is abnormal either in intensity or focus B) apparently inflexible adherence to specific, nonfunctional routines or rituals C) stereotyped and repetitive motor manners (e.g., hand or finger flapping or twisting, or complex whole-body movements) D) persistent preoccupation with parts of objects
B. Delays or abnormal functioning in at least one of the following areas, with onset prior to age 3 years: (1) social interaction, (2) language as used in social communication, or (3) symbolic or imaginative play.
C. The disturbance is not better accounted for by Rett’s Disorder or Childhood Disintegrative Disorder.
If you do not feel that your child meets at least six of the criteria listed here, you may want to look at the criteria for other disorders on the “autism spectrum.” Click here to read about Asperger Syndrome, Pervasive Developmental Disorder, Rett’s Disorder, and Childhood Disintegrative Disorder.
Still Worried?
If you are concerned that your child could have autism and he or she does not have a diagnosis, discuss your child’s differences with an experienced pediatrician, developmental pediatrician, neurologist or psychologist who is qualified to make an official diagnosis. You can also/simultaneously request a free evaluation for autism through the regional center, which may lead to eligibility for services after the age of three for your child. (More information is provided about this option on this site). Your understanding of the features of autism, along with concrete examples from your child’s daily life, will help a qualified diagnostician identify autism.
You can ask your pediatrician to do a developmental screening, using a tool like the M-CHAT (Modified Checklist for Autism in Toddlers) for children from 16 to 30 months of age. A formal screening tool like the M-CHAT includes parent input and may be a good choice to gauge a young child’s development.
Developmental screening is as important as screening for physical development, hearing, or vision. In fact, the American Academy of Pediatrics policy is that every child in America should have developmental screening at the 18 month and two year well-baby visits. This helps the doctor notice particular differences that can indicate autism and make a referral for further evaluation.
Sometimes doctors do not offer to do the M-CHAT or other developmental screenings. However, if parents ask for it, the child can have the screening, especially if there are any concerns about socialization, communication or play skills. You will want to ask for the M-CHAT or a similar screening tool for any younger siblings of your child with autism. M-CHAT en Español.
Reacting To Your Childs Diagnosis
When your very young child is diagnosed with autism, coming to terms with this reality can be overwhelming. You may feel so many emotions- crushed, confused, lost, or even angry. You may be grieving or “in denial” and not want to believe that it is true. You need support to deal with these reactions.
At the same time, we encourage you to be hopeful about your child’s future. There are many ways to help children with autism learn, progress and realize their potential. Identifying autism early means that services can start early. Aim high and dream big for your child. Then, work hard to be sure that your child gets what he or she needs to realize the dreams you have for your child, and his or her own dreams.
Some parents actually are relieved to get a diagnosis. They consider a diagnosis an accurate explanation of their child’s differences. It may be an official confirmation of a parent’s intuitive understanding of differences seen all along. Click here to explore more on this topic.
Next Step: Navigating The System
The next step after diagnosis is to identify your child’s needs and work with any provider or service system that can help meet those needs. There is help out there for you! Individuals, organizations, and agencies know what kind of therapies and treatment can help, and how to get that help. Some service systems also consider the needs of parents, family members or others taking care of the child with autism.
You may work with several different agencies or providers to secure all the services your child needs. Three main providers for young children from birth to age 3 in California are the regional center, health insurance, and the school district. The section below describes these three options. It is possible that your child can receive services from two or more of these systems. You may work with private services providers as well.
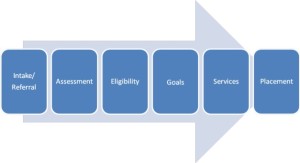
There is usually a common way to enter any service system, or Navigate the System. The procedure you can expect is represented by this graphic:
To help you understand how to navigate the service systems you will be encountering, let’s start with a system you know, the healthcare system. If your had weakness in your right arm, you would go to a doctor to explain what was wrong. You are starting the process yourself. This is called self-referral. Your doctor would listen and then refer you to an orthopedic specialist. Think of a referral as the way to get in the door to the person who can help you.
The specialist would start with testing or assessment. Assessment gets to the bottom of what is going on and defines what you need. After testing, the specialist may confirm a diagnosis and tell you that you need some type of treatment. This is like the stage of eligibility: it is confirmed that your condition qualifies you to receive services/treatment.
The specialist would then make a goal: to regain normal functioning of your arm. The goal spells out what are you trying to accomplish. The specialist may prescribe physical therapy as the service you need to meet the goal. You would find a local service provider where therapy can take place, this is like a deciding on a placement.
You will find that the service systems you encounter now and in the future generally follow these six steps of referral, assessment, eligibility, goals, services and placement. Even if your child has already been evaluated to receive a diagnosis, more assessments are usually conducted to understand the child’s level of functioning in different areas of need: social, communication, adaptive behavior, motor skills and thinking/learning (also called cognitive), or any area of concern for a particular child.
Assessments are the KEY to services. Why? Goals are only written and services are usually only provided in areas that have been assessed in some way! No assessment, no goals, no services.
The Service Systems
Information in this section can help you understand the service systems that may be involved in the care of a child near the age of 3. When your child is under age 3 there are two main service systems you need to know about:
Early Start through the Regional Center
Medical Insurance
If your child is age 3 or older, these are the three main service systems you need to know about:
Regional Center
Insurance
School District
Read on to learn about what to expect and how to navigate these systems.
Regional Center
Regional centers are nonprofit corporations operate under contract with the California Department of Developmental Services (DDS). Regional centers provide and coordinate services and supports for individuals with developmental disabilities in California. There are twenty-one regional centers. Seven of them are located in Los Angeles County, serving specific areas within the county.
Click here for a list of regional centers near Los Angeles and the areas they serve.
Insurance
Your private health insurance may cover some services that your child needs. The key to receiving services through your insurance company is determining that the services are “medically necessary.” Each insurance company in California is currently allowed to determine what is or is not medically necessary; there is no state standard for this. Many decisions are made on a case-by-case basis. This means you will have to find out what types of services your policy covers, the policies of your insurance carrier, and discuss your child’s unique case with your medical provider.
Your child’s doctor can take the lead in prescribing services for your child and using specific provider codes to help with the process. Some families are pleasantly surprised to find out about the services that may be covered. Other families find this an area of struggle.
Several states have passed legislation requiring all insurance carriers to provide specific services related to autism. In spite of many efforts, California is not one of these states. You may want to be aware of the progress of insurance legislation in California and do what you can to help bring consistent quality medically-related services and care to individuals with autism to California.
Here are SOME of the medically necessary services relevant to children with autism from age birth to three covered by SOME insurance carriers. Remember to find out what your policy covers and the policies of your insurance carrier.
Diagnosis
Parent Training
Feeding Therapy
Speech Services
Occupational Therapy
Physical Therapy
Applied Behavioral Analysis / Behavior Intervention Services
If your child is denied a service that your child’s doctor feels is medically necessary, there is an appeal process in the insurance system.
The Early Start System For Children Under Age 3
Regional Center Programs and Services
Regional Centers have several programs for infants and toddlers. Please read all of this section to find the one that may be right for your child.
Regional centers administer a special program called Early Start, which is a type of early intervention service for children from birth to age three who have delays. The goal of Early Start is to find and help young children who need support or services to develop. Because the Early Start program is funded by the federal government, it is has its own unique criteria for eligibility. No formal diagnosis is needed to provide services for the child and family.
If your child is under the age of three and has noticeable delays or has autism, you will want to get free Early Start services for your child. You don’t have to wait for your child’s third birthday to get help, and you don’t have to wait for confirmation of a diagnosis from your pediatrician to get the process started.
Early Start services are accessed by starting “intake” with the regional center to find out if your child is eligible. Children under age 3 who do not qualify for early start may qualify for a different regional center program called the Regional Center Preventative Program.
Useful publications for Early Start programs for children under age 3.
Regional Center Preventative Program
Early Start Eligibility
Early Start Appeal
Early Start
When you have noted significant differences in the development of your child from the age of birth to 36 months, your child may be eligible for Early Start services from the State of California.
What is Early Start?
Early Start is the name of the special program for early intervention services in California. Early intervention services are designed to support the development of infants and young children under the age of 3 who are showing delays. Early intervention services are intended to help narrow or close gaps in development for children related to concerns in areas such as:
Developmental Delay (not meeting expected milestones of growth, development)
Adaptive, Self-Help (not meeting milestones of daily functioning or skills)
Communication (not talking or communicating as expected for his age)
Social-emotional (not relating or bonding with others, not responding to the people and things in their environment as expected)
Cognitive (may have impairment in thinking or learning)
Physical (has difficulties affecting the muscles, nervous system, or parts of the body)
In addition, children with certain risk factors may also be served in the Early Start program:
Established Risk (child’s parents have a risk factor such as cognitive or developmental delay)
Low-incidence (risk factors that occur infrequently, such as visual impairment)
High risk (genetic or known risk factors that impact a child’s development)
In Early Start, infants or toddlers are assessed or evaluated. The Early Start system has specific criteria for eligibility, and often no formal diagnosis is required in this system.
Children found eligible can receive early intervention and family support services until the third birthday. The federal government and state provide the funding for Early Start programs, so that needed services are provided to the children who need them, using insurance funding or public funds.
In California, the regional center is the main point of contact for Early Start services. The regional centers also offer a Preventative Program for some children who do not qualify for Early Start. Talk this over with the regional center staff if it is relevant to your situation. Click here to find a Regional Center near you.
Many times the symptoms of autism are not recognized until the second year of life. Many children who have autism or who have signs of autism will not be part of the Early Start system because by the time many families are ready to enter Early Start, their child is nearly three. If your child has early signs of autism or is diagnosed early, be sure to take full advantage of the developmental services available through Early Start. It can be difficult and frustrating for those new to the Early Start system to have to move to new services and providers through other systems after only a few months, but it may be worth it!
Finishing the Early Start program on the child’s third birthday does not mean your child is also “finished” with the regional center! Once your child turns three, he or she may continue to receive needed services through the regional center (just not through the Early Start program).
The process of enrolling your child in the Early Start program is similar to the process of navigating any service system. See the graphic below to get an idea of what to expect:
Graphic representing the assessment path for autism.
^Top
Who makes the referral for Early Intervention Services?
Anyone can make a referral for early intervention services through the Early Start program, including parents, medical care providers, neighbors, family members, foster parents, and day care providers. You may have been told about Early Start by your child’s doctor or pediatrician when discussing concerns about the child.
To start the process, call the local regional center, tell them that you have significant concerns about your young child’s development, and request an Early Start evaluation for the child.
What happens after a referral: The Intake Process
The “intake” process for Early Start is 45 days from start to finish, starting with the day of your call. In that time frame, the regional center will:
Assign a service coordinator to assist you through the evaluation and assessment procedures.
Obtain your consent to evaluate your child.
Schedule and complete evaluations and assessments focused on child development.
Determine if your child meets the eligibility criteria for the Early Start program
Develop an Individual Family Service Plan (IFSP) that addresses the strengths and needs of eligible infants or children and their family. The IFSP includes parent concerns and determines what early intervention services are
Identify early intervention services to be provided in the family home or other community settings, link the family to those services, and pay for the services.
^Top
Assessment
Teams of service coordinators, healthcare providers, early intervention specialists, therapists, and parent resource specialists evaluate and assess infants or toddlers. Assessment usually includes interviews with parents and observation of the child, along with other age-appropriate diagnostic testing. Assessments are done to identify developmental delays in the following areas:
Cognitive (thinking and learning)
Communication (speech, language, non-verbal communication like gestures, nodding)
Social and emotional (relating, interacting, playing, self-control, etc.)
Adaptive (how the child functions on a daily basis)
Physical and motor (muscles/coordination development, including vision and hearing)
^Top
Who Is eligible?
Infants and toddlers from birth to 36 months may be eligible for early intervention services in the Early Start program. The decision is made based on the assessment results, the age of the child, and particular concern about the significance of the delay. The child must meet ONE of these three formal criteria for eligibility:
Be under 24 months (2 years of age) at the time of the referral and have a 33% delay in one or more areas of development.
Be 24 months (2 years of age) or older at the time of referral, with a 50% delay in one area of development or a 33% delay in two or more areas of development.
Have an established risk condition of known etiology (cause), with a high probability of resulting delayed development. An examples of this kind of risk is having Fragile X, a genetic condition likely to result in developmental disability.
The older a child gets, percentage of delays must be greater than for a younger child, and more areas need to be affected in order to qualify for Early Start services. Click here for visual model of this information.
^Top
What if Early Start eligibility Is denied?
If eligibility for Early Start is denied and you disagree with the denial, there is a process for resolving the disagreement. The denial letter will include the paperwork and instructions to appeal the denial or file a complaint. See Early Start Appeal PDF.
In this process, you will briefly state the issue(s) related to the disagreement and describe what you believe to be the appropriate solution to your disagreement.
Once a complaint is filed, there are two processes available at the state level to resolve your dispute. One is a voluntary mediation conference, an impartial and non-adversarial dispute resolution process. The second option is a due process hearing.
The parties to the disagreement are encouraged, as a first step, to utilize the mediation process. To request a Mediation Conference, complete form (DS1808) Mediation Conference Request. If mediation is not successful in resolving the issue(s), the parties automatically proceed to a due process hearing.
^Top
Goals and Services in the Individual Family Service Plan (IFSP)
Once the child is assessed and found eligible, an Individualized Family Service Plan (IFSP) is designed to describe the areas of need and agree upon the services to be provided. The IFSP is “family-centered” and includes services and supports for the child and the parents. The Individualized Family Service Plan is required by the Individuals with Disabilities Education Act (IDEA) for all infants receiving early intervention services.
The IFSP is written by your service coordinator or case manager with your input. Those who assessed your child, such as an infant educator, physical therapist, occupational therapist, or speech and language therapist can also participate in creating the IFSP. The people who design and implement the IFSP are called the multidisciplinary early intervention team, and parents are part of the team.
The IFSP is written in the form of a report. It is a confidential document, meaning that the information is shared only as needed with those involved in the plan. If a situation arises when it is necessary to share information with someone outside of the team, your consent is required.
The IFSP document may be organized as follows:
1. Description of the family and child: This includes the family composition (who the child lives with, where, if there are brothers and sisters, etc.). A physical description of the child and a brief description of his or her skills, behaviors, or concerns are included.
2. Family Priorities: The family is helped to explore and describe what concerns them the most, and what they would like help to work on, for the child and family.
3. Family Resources: Families may choose to discuss the resources that they do or do not have available to them, such as health insurance, etc.
4. Eligibility: Reasons for the child’s eligibility are described, including specific concerns or delays in one or more of these areas:
Developmentally Delayed (not meeting expected milestones of growth, development)
Adaptive, Self-Help (not meeting milestones of daily functioning or skills)
Communication (not talking or communicating as expected for his age)
Social-Emotional (not relating or bonding with others, not responding to the people and things in their environment as expected)
Cognitive (may have impairment in thinking or learning)
Physical (has a disability affecting the muscles, nervous system, or parts of the body)
High Risk (genetic or known risk factors)
Established Risk (child’s parents have a risk factor such as cognitive or developmental delay)
Low-Incidence (risk factors that occur infrequently, such as visual impairment)
5. Reports of Developmental Status and Health Status: A comprehensive assessment of the child’s development and health is done to determine if the child is at risk or in need of early intervention. These assessment results reflect the child’s present levels of functioning and health, and are part of the IFSP.
6. Outcomes: In the IFSP, goals for the child and family are called “outcomes.” These are based on the priorities of the family and related directly to the services needed to result in those outcomes.
7. Services: The specific early intervention services needed to meet the goals (including the frequency and intensity and method of delivering services, the projected date of initiating services and the anticipated duration of services) are specified in the IFSP.
8. Transition Plan: If it is likely at age three that the child will require special education services, a transition plan should also be stated in the IFSP. This means that you will receive assistance to transition to services for children from the age of three and up, whether they are provided by the regional center or the school district.
9. After the IFSP is written and agreed upon it becomes a contract between the Regional Center and the family. Services should be delivered as outlined in the IFSP. The IFSP should be evaluated and adjusted at least once a year and reviewed at least every six months. For more information, see “Part C” of IDEA (Individuals with Disabilities Education Act) that relates to early intervention services and creating the IFSP.
^Top
What early intervention services are available?
Based on the child’s assessed developmental needs and the families concerns and priorities as determined by each child’s Individualized Family Service Plan (IFSP) team, early intervention services may include:
Assistive Technology
Audiology
Family Training, Counseling, and Home Visits
Health Services
Medical Services for Diagnostic/Evaluation Purposes Only
Nursing Services
Nutrition Services
Occupational Therapy
Physical Therapy
Psychological Services
Respite Services
Service Coordination (Case Management)
Social Work Services
Special Instruction
Speech and Language Services
Transportation and Related Costs
Vision Services
^Top
What other services or resources are available under Early Start?
Families of infants and toddlers, from birth up to 36 months can also receive parent-to-parent support from Family Resource Centers, or FRCs. The mission of the FRC is to support children with special needs, children at risk, and their families. FRCs are family-centered and parent-directed. They are usually staffed by experienced parents who have children with special needs. This may make the staff particularly qualified to provide information and parent-to-parent support.
FRC’s may be “stand alone” Early Start FRCs, that only help parents of children up to age 3 access early intervention services. Other FRCs have Early Start specialists who assist families with children from birth to age three, as well as staff who can continue to assist families of children from age 3 to 22.
Each FRC is unique, reflecting the needs of the community. FRCs actively collaborate with local regional centers and educational agencies. FRCs may operate as independent sites.
They can also be based in regional centers, local education agencies, public health facilities, hospitals, or homes. Services are available in many languages and are culturally responsive to the needs of families.
FRC’s may provide these services related to Early Start:
Parent to Parent and Family Support
Peer Counseling and Home Visits
Information and Referral
Public Awareness
Parent Education
Support Services in Many Languages
Transition Assistance at Age 3
Support Services in Urban and Rural Communities
Some family resource centers have newsletters, a resource library, a website, parent support groups, sibling support groups, and telephone warm lines. Visit the FRCNCA website for more information: http://www.frcnca.org
^Top
Who provides services? Where are services provided?
Early intervention services that are needed for each eligible infant or toddler are purchased or arranged by a regional center. The case coordinator will provide lists of potential service providers in each area of need, and the family usually has the option to choose which provider to use.
How much does it cost?
There is no cost for evaluation, assessment and service coordination. Public or private insurance is accessed for medically necessary therapy services including speech, physical and occupational therapies. Services that are not covered by the family’s insurance will be purchased or provided by regional centers.
What happens at age 3? Transition between Regional Center and School District.
Early Start services end at the age of 3, usually on the child’s third birthday. Finishing the Early Start program does not mean your child is also “finished” with the regional center! Once your child turns three, he or she may continue to receive needed services through the regional center (just not through the Early Start program).
At age 3, children who received Early Start services can also transition to receive services form the school district and/or a different “department” within the regional center system. Evaluations are done to help with this transition and offer appropriate, comparable services in the new service system. Be sure to work with your child’s case coordinator to make a smooth transition, as well as rely on the resources at the Early Start Family Resource Center.
^Top
Timeline For Transition To Pre-School Age Services
Here is a recommended timeline to ensure that your child is ready to start their school program on his or her third birthday as required by law AND continue to receive needed services through the Regional Center after the third birthday.
When your child is 30 months old: Your Regional Center service coordinator should facilitate an introduction meeting for you to meet with a school district service coordinator. If your Regional Center does not facilitate this meeting, ask your coordinator for the contact information so that you may begin the process of preparing for your first IEP (Individualized Education Plan) meeting.
When your child is 31 months old: You should receive an assessment plan from the school district to evaluate your child. If you do not receive an assessment plan, request one in writing from the school district. The district has fifteen days from the receipt of your written request to issue an assessment plan. Upon receipt, you have fifteen days to review the plan.
Be sure that assessment in all areas of functioning are included in the plan. Why? Goals are only written and services are usually only provided in areas that have been assessed in some way! No assessment, no goals, no services.
Remember, if you have reason to believe that your child will need behavioral intervention from the school district to meet his or her educational needs, the assessment include a plan MUST to conduct a Functional Analysis Assessment (FAA) by a qualified person trained in behavioral assessment, at your request.
Review the assessment plan carefully. You may want your case manager, someone from an FRC or someone else to review it before you sign that you agree with the plan. Assessments are the KEY to services. If something is missing, ask that it be added to the plan. Once you agree with the assessment plan, sign and return it to set the timeline in motion for the assessment process.
When your child is 32 months old: Ask your Regional center service coordinator to start the evaluation process to determine if your child can continue to receive services through the Regional Center after the age of three. If he or she tells you it is too soon to ask, find out when you can make the request and put it on your calendar to follow through.
If you would like to have an advocate or an attorney help you with the IEP process and/or attend the IEP meeting, you should contact them at this time to help them get to know your concerns and become familiar with your child’s case. Compile any assessments from service providers who are currently working with your child.
When your child is 34 months old: Take your child to assessment appointments with the school district AND the Regional Center.
Work with your Regional Center service coordinator to set up the date for the IEP (Individualized Education Plan) meeting. Invite your child’s current service providers and your Regional Center caseworker to attend the IEP with you. Notify that school district that you will need to receive the school’s evaluation report and proposed goals at least 5 days prior to the IEP meeting.
When your child is 35 months old: Follow through with your Early Start case coordinator to find out if your child was found eligible to receive Regional Center services after the age of 3. You cannot continue with your child’s Early Start case manager after your child turns three; he or she will tell you who your new case manager will be. Contact this person to set up the IPP meeting to discuss needs, goals and services for home and community.
If your child is NOT found eligible to continue Regional Center services after age 3, you will receive a written notification by mail. If your child is denied, you can appeal the denial; paperwork and instructions will be included with the denial letter. Send in your appeal paperwork within 30 days of receiving your letter to start the process to resolve the issue.
About two weeks prior to your IEP, gather important records and documents. Organize and review evaluations and progress reports from current service provider’s and any doctors’ notes or recommendations that may be valuable. Make a list of “Parental Concerns,” describing areas of your child’s development, functioning and behavior that you wish to have addressed in the IEP meeting and in your child’s educational program. You may even create a list of suggested goals for your child, and services you feel are necessary to achieve these goals, and provide this list to the school district in writing.
The week before your first IEP meeting: Be sure you have received the school assessment reports least 5 days prior to your IEP to give you time to review the results. You may want to ask your Early Start providers to explain the results to you so that you understand all of the scores and results.
Let the school district coordinator know if you are bringing an advocate to your meeting. If you wish to tape record the IEP meeting, you will need to give written notice 24 hours in advance.
Eight KEY Points Regarding the End of Early Start Services
1. Early Start is an early intervention program funded by the federal government that is administered by the regional center. The regional center has a different program for individuals from age 3 through the lifespan that your child may be eligible for when Early Start ends.
2. Your child can receive many supports and services for home and community through the regional center after age 3, possibly including in-home behavioral services. A new assessment or record review will be required to determine needs and eligibility.
3. The regional center will usually not offer to do this assessment! The assessment for continued services is usually done only at YOUR request. Be sure to ask for the regional center assessment 3 to 4 months before the third birthday.
4. The Early Start coordinator can/should assist you setting up an assessment to determine if your child can remain a client of the regional center. This usually includes diagnostic evaluation for autism, whether your child is already diagnosed, or if autism is suspected.
5. Be sure to request the regional center evaluation and follow through to ensure that your child receives this assessment for continued regional center service. Your child will automatically be “exited” from the regional center system and your child’s case will close on the third birthday UNLESS the assessment is done to determine eligibility after age 3.
6. The regional center system typically only finds children eligible who are found to have “autism.” If you usually call your child’s autism by another name (like Asperger syndrome, PDD, etc.) remember to talk about “autism” in formal situations.
7. Part of the assessment for continuing with regional center services after age three is determining if your child has significant impairment due to their autism in at least three of the following domains that are relevant to children of his age: self care, receptive and expressive language, learning, mobility, and self-direction. Notice and think about the ways your child is affected by autism in a daily basis, and be sure to share this information.
8. If your child is currently enrolled in Early Start through the regional center, your Early Start case coordinator must assist you in making the transition to the school district, by law!
Special Education for Pre-School Age Children
Many children with Autism Spectrum Disorders or suspected autism are found eligible for early intervention services (called Early Start in California) somewhere around age 2 1/2. This may mean that your child has recently been evaluated and has just begun Early Start services when “suddenly” the child’s third birthday approaches and you are notified that Early Start services must end. It is very likely that your child will still need services after he or she turns three. What happens when Early Start ends?
flowchart of early start program
At age 3, services and supports for your child CAN continue, but responsibility is shared between the school district AND the regional center. There are steps you need to take to ensure that this change happens as it should, and there is help for you in the process.
Pre-School Education After Early Intervention
Special consideration: If a child received Early Start services, the program they receive from the school system should be comparable.
Families are often dismayed to find they must make a change just when they have learned to “navigate the system,” understand what to expect, and develop relationships with staff. This “move” can be very stressful for the child and family. IDEA law states that the transition should be made as smoothly as possible.
To do this, early intervention staff and other specialists who have worked with the child, and know her well, need to be involved in developing the pre-school education plan. School districts can be open to the needs of the family to continue to use services already in place whenever feasible, and when necessary, find new services that are suitable and comfortable for the child and family. Districts should also try to be as clear as possible to help parents understand how their “system” works and what to expect.
KEY POINTS in thinking about this shift in the service system:
The program and services your child receives starting at age 3 should be comparable to what he or she is receiving in receiving Early Start. Based on his or her needs, a combination of school district and regional center services can maintain the type and amount of services your child is receiving through Early Start, at home and in an educational setting. Even though services are split between two different agencies, it is important to “keep the child’s program whole.”
When making decisions about the new preschool-age services and programs, you want to ask yourself, “Are we keeping my child’s program whole?” You can even ask this question out loud when working with agency staff and support personnel to be sure that your child’s needs continue to be met. Decisions must be based on the needs of the individual child.
Example 1: Your child with autism was receiving 1 hour per week of individual physical therapy in Early Start to promote coordination and strength. How do you keep this whole when your child transitions to preschool? Here are some possibilities:
The district agrees to provide 1 hour per week of individual physical therapy (perhaps in a clinic).
Your child continues receiving 1 hour per week of individual physical therapy through your health insurance, and you take the concern out of the IEP arena.
Your child is assessed by the school district in the area of Adapted Physical Education (APE). Needs are determined, and the child receives 90 minutes per week of group adapted physical education to learn to move safely around the school and access all of the playground equipment (thus building strength and coordination).
Example 2: Your child received 1 hour per week of individual speech and language services in Early Start, and 1 hour of group child development per week, and made slow progress. Now the district is offering 30 minutes per week of group speech, and placement in a “language rich” preschool program 16 hours per week. Is what the district is offering comparable to the level and type of service your child had? Probably not. The answer depends on your child. Your early intervention service providers may be able to help you decide on that. Progress reports and assessments that have been done in the area of speech and language may also shed light on whether 30 minutes of group speech would be adequate to meet the child’s needs and help them reach their goal for the next twelve months.
Example 3: Your child received 25 hours per week of services in Early Start that included 5 hours total of individual and group therapy, and 20 hours of in-home discrete trial training.
Now the school district is offering 3 hours a week total of individual and group therapy, and a 16 hour special education preschool program. How can you keep your child’s program whole? One answer is to have the regional center provide in-home discrete trial training in addition to the school-based program. This would be agreed upon outside of the IEP meeting, in a separate meeting with the regional center. Your Early Start case manager can help facilitate this type of cooperation and coordination of services.
If you have reason to believe that what the district is offering in the IEP is not comparable to the services that enabled your child to progress in Early Start, point this out and ask them to keep the goal of comparable services in mind. The district will usually try to work to fix the discrepancy. If the district’s final offer of services is not comparable or adequate in your view, you can disagree with the offer and take steps to resolve the disagreement.
Please see “Who is Eligible for Early Start services?” Available here.
Regional Center Services After Age 3
The regional center may also provide services to eligible individuals with developmental disabilities from age three and up. Developmental disabilities include mental retardation, cerebral palsy, epilepsy (seizure disorders), autism, and other conditions closely related to mental retardation, that require similar programming. To be served by the regional center, the person’s disabling condition must originate before the age of 18, be expected to continue indefinitely, and must constitute a substantial handicap for the individual. (Conditions that are exclusively physical impairments are not considered developmental disabilities).
What kinds of services are available through the regional center?
The regional center provides services and supports to help the person with a developmental disability (called the consumer or client) with focus on meeting needs at home and in the community. The regional center serves clients from age three and up, and may continue to serve adults, or even senior citizens, if services are required.
A wide variety of services are available, depending on the needs of the consumer in various domains. Examples include assessment for the diagnosis of autism, in-home behavioral therapy, specialized day care, specialized after-school care, social skills instruction, recreational therapy, support staff to help the client access the community, etc. Parents or caregivers may receive respite services (to get a break from the intensive care needs of the child) and parent education (to learn to assist and advocate for their children).
The regional center cannot provide any service that another agency is responsible for providing. The regional center is the provider of last resort, and usually only provides services if insurance and “generic community resources” (other options available to you) have been exhausted. For example, the regional center would not provide educational services for a school-age child whose educational needs should be met by the school district, or medical services for someone who has insurance coverage for the service.
To learn more about the types of services your child may need, please go to New to Autism > Autism Therapy & Treatment.
Is there a cost?
Many services provided through the regional center are at no cost to the consumer or their family. Other services may have a “parental share of cost” based on household income.
How Can My Child Become a Regional Center Client
If your child has autism, the regional center can be an integral part of meeting your child’s needs, now and in the future. The regional center system requires the expected six steps to enter the system: intake/referral, assessment, eligibility, goals, services and placement (deciding the places where services will be provided).
autism-path
Referral and Intake
The process of intake or referral starts with your phone call to the regional center office located in the area where you live. You don’t need anyone’s permission or instructions to call! Ask to speak to the “Intake Officer of the Day.” State that your child has a diagnosis of autism and you would like to begin the intake process. Or, if your child does not have a diagnosis, explain that you suspect your child has autism or a developmental delay and you would like to start the intake process.
In either case, the regional center will set up two appointments with you. The first appointment is typically an interview with an intake officer (usually a social worker), who asks you questions to determine if it is likely that your child has autism. Your child does not have to be present for this appointment.
The information you share at this meeting is carefully considered. You may want to write down your concerns and give specific examples of things that your child does or does not do that you have noticed. You can even use the two checklists from this website to help you organize your thoughts. Be sure to describe how your child’s difficulties impact his or her functioning on a daily basis.
At the meeting, you can provide the checklists or other summary in writing that clearly presents your concerns. You may also be instructed to bring copies of any relevant formal records about your child to this meeting, like a diagnosis you have obtained already, notes from the pediatrician, etc. This helps the intake personnel gather needed information.
If there is enough evidence of autism or suspected autism, a second appointment will be made for your child to be evaluated by a regional center psychologist (and sometimes, a team of evaluators). The information from your intake appointment will be shared with the evaluator(s). The evaluator will do testing with your child in a variety of areas (cognitive, developmental, diagnostic, physical, etc.). You will also be interviewed and asked to fill out questionnaires about how your child functions in areas like socialization, communication, behavior, self-care, etc.
The regional center psychologist will write a report about your child. It usually includes a summary of all the information that was shared, along with findings and scores from the evaluation process. The report will describe the features of autism that were seen in your child. The report will describe features of autism that were NOT seen in your child.
The information in this report is used by the psychologist to determine eligibility whether or not your child will become a client of the regional center to receive needed services. There are two parts to this decision. The first part is whether your child has at least 6 of 12 features of autism. The second part is whether your child has a substantial handicap as a result of the autism. In the case of a young child with autism, substantial handicap means that the features of autism affect the person significantly in three or more domains of functioning on a daily basis, such as socialization, self-help or adaptive skills, receptive and expressive language, learning, access to the community, and self-direction.
If your child is found eligible, you will receive a confirmation letter in the mail. Your child’s report will include assessment results that confirms the diagnosis and eligibility. Within a few weeks, a case manager is assigned, and an IPP Meeting (Individualized Personal Plan) is held to determine the needs of the client, write goals, and agree on and the services and supports.
Click here to learn about important considerations for regional center eligibility for individuals age three and up.
If your child is not found eligible for regional center services, you do not have to accept the denial. There is an appeal process. You can take steps to gather more information and resolve the disagreement through mediation or due process. If you win your appeal, your child will become eligible for regional center services.
Click here for more information about the appeal process.
The Early Start System For Children Under Age 3
- Transition Handbook
- Early Start Brochure
- Early Start Denial Appeal
- Early Start Eligibility Visual Model
- Family Resource Centers Network of California
- Los Angeles Regional Centers
- M-CHAT
- M-CHAT en Español.
- Picture Dictionary Checklist
- Picture Dictionary of Child Development
- Reacting To Your Child’s Diagnosis
- Regional Center Preventative Program
- DSM 5 criteria for Autism Spectrum Disorder and Social (Pragmatic) Communication Disorder.